
The Pfizer/BioNTech COVID-19 vaccine, trade name Comirnaty.
As we’re now three years out from the beginning of the pandemic, there’s a lot of information emerging about our behaviors from one or two years ago. Given the demonstrable benefits of COVID-19 vaccination, it’s important to understand the reasons for declining the vaccine. Two weeks ago I looked at a study examining the use of ivermectin and hydroxychloroquine, and the relationship with endorsement of misinformation, or of lack in trust in scientists and physicians. Today I want to look at reasons for vaccine refusal in an non-American population – in this case, Hong Kong.
Background
Pre-vaccine, Hong Kong was regarded as having a strict but effective pandemic response. Its containment strategy failed as the more contagious Omicron variant took hold in 2022, and swept through a population that was poorly vaccinated. At that point, 82.4% of adults aged 80 and older were either unvaccinated or had received only one dose. By, comparison, these rates were 2.9% in New Zealand, 9.0% in Singapore, and 6.7% in England. Hong Kong subsequently experienced the highest daily COVID-19 mortality in the world, with 39.3 deaths per million people. While Hong Kong’s overall COVID-19 death rate per capita is lower than that of the UK and US, it has surpassed many other countries in the Asian-Pacific.
One hypothesis for the low vaccination rate was the fact that there were few or zero COVID-19 cases for extended periods, which could have led to complacency. However, low or zero COVID was achieved in other countries (e.g., Singapore, Australia, New Zealand) which subsequently had high vaccination rates. A more unique factor could have been the social and political changes that had occurred in Hong Kong related to a proposed extradition bill which divided Hong Kong residents and led to mistrust of officials (for some). In short, the extradition bill would allow Hong Kong to extradite criminal suspects to China (or any other country), even countries for which it didn’t have an extradition treaty. The bill was met with massive protests in Hong Kong. Groups like Amnesty International, Hong Kong Human Rights Monitor, and Human Rights Watch all voiced opposition to the bill.
This study, from Phylllis Lun and colleagues, which was published in JAMA Open on October 19, 2023, leveraged data from 20 waves of data from a prospective cohort study. It also drew upon a population-wide registry of all COVID-19 vaccination appointments. The researchers sought to measure the progression of willingness to get vaccinated into actual vaccine uptake. They also investigated the factors influencing the rejection of COVID-19 vaccines, and the overall effect on the population.
Patients were drawn from an ongoing population-based cohort study which had recruited over 18,000 adults and adolescents (>15 yrs). This study sampled just over 1000 from that group several times between 2020 through 2022. Response rates were good, at about 75%. The researchers also compared Hong Kong findings with a sample drawn from Singapore. Willingness to vaccinate against COVID-19 was assessed as receiving at least 1 dose of vaccine, making a vaccination appointment, or expressing an intention to vaccinate. COVID-19 vaccine refusal was defined as having no intention to receive COVID-19 vaccines. Political views were assessed as whether participants were “for, against or neutral” towards the extradition bill, which were classified as “proestablishment, nonestablishment, and neutral”, respectively. Trust in vaccine information sources was assessed by asking about the level of trust in the World Health Organization (WHO), government health authorities, physicians, academics, and traditional and social media platforms as information sources for COVID-19 vaccines. Vaccine confidence was assessed using 3 statements on the perceived effectiveness, safety, and importance of COVID-19 vaccines:
- COVID-19 vaccines are effective
- COVID-19 vaccines are safe
- COVID-19 vaccines are important for children to have
Findings
Overall, an amazing 28,000 interviews were conducted.
Vaccination willingness – from before rollout to mass vaccination
In 2020 (pre-vaccine), around two-thirds (65%) of adults in Hong Kong expressed a willingness to get vaccinated once a vaccine became available. This willingness increased to 73% in response to positive COVID-19 vaccine trial outcomes, and a local outbreak. However, when the Hong Kong government announced the procurement of vaccines from Germany, mainland China, and the United Kingdom, with individuals not having the option to choose their preferred vaccine (though this decision was later reversed after 12 days), the willingness to vaccinate dropped to 55%. The launch of the vaccination program and a surge in media reports regarding adverse events following COVID-19 immunization were accompanied by a decline in vaccination willingness, reaching its lowest level at 44%:
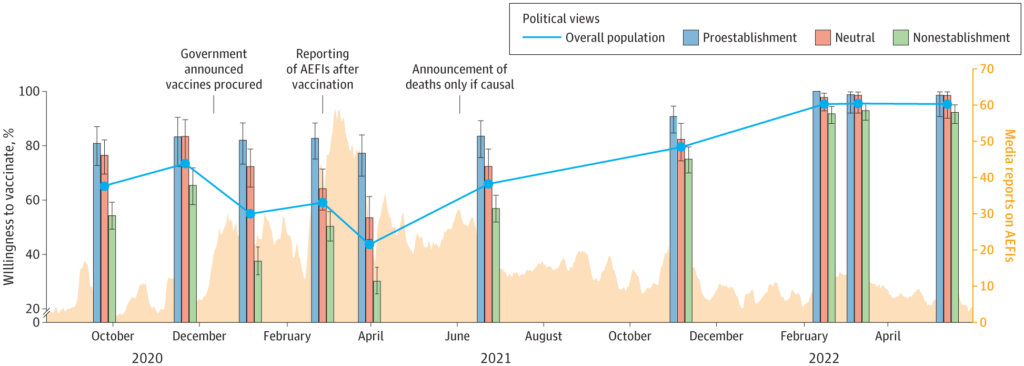
Figure 1. Trends in Vaccination Willingness and Media Reports on Adverse Events Following COVID-19 Immunization (AEFIs)
The authors looked at the daily numbers of vaccine appointments over time. They noted that in adults aged 18-59, workplace vaccine mandates were associated with an increase in daily COVID-19 vaccination appointments by 74% and the vaccine pass in Hong Kong was associated with an increase of 131%. Vaccination appointments increased by 44% during the Omicron surge. However, lottery-based incentives were not associated with changes in vaccination appointments. In older adults (age ≥60 years), the vaccine pass was associated with a 94% increase in vaccination appointments, and subsequent reopening of premises under the vaccine pass was associated with an 112% increase. Similarly, the Omicron surge was associated with an increase in vaccination appointments (107%). Lottery-based incentives and workplace mandates were not associated with changes in vaccination appointments among older adults:

Figure 2. Daily Appointments of COVID-19 Vaccination (Primary Series) for Individuals Aged 18 to 59 Years (Top Panel) and ≥60 Years (Bottom Panel)
Factors Associated With COVID-19 Vaccine Refusal
Individuals holding “nonestablishment” political beliefs were more likely to refuse the COVID-19 vaccine when compared to those with “proestablishment” views among adults aged 18 and older (adjusted incidence rate ratio, 3.26 [with a 95% confidence interval of 1.63-6.51]). This was also observed in adults aged 60 and older,but to a lesser extent (adjusted incidence rate ratio, 2.10 [95% CI, 1.15-3.83]). Levels of trust in sources of vaccine information, confidence in vaccines, and misconceptions about vaccines differed based on an individual’s political views:

Figure 3. Trust in Information Sources, Vaccine Confidence, and Vaccine Misconceptions, June to July 2021
The study also found that political involvement during the 2014 “Occupy Central protests” was associated with a higher likelihood of COVID-19 vaccine refusal.
Vaccine Misconceptions and Trust in Vaccine Information Sources
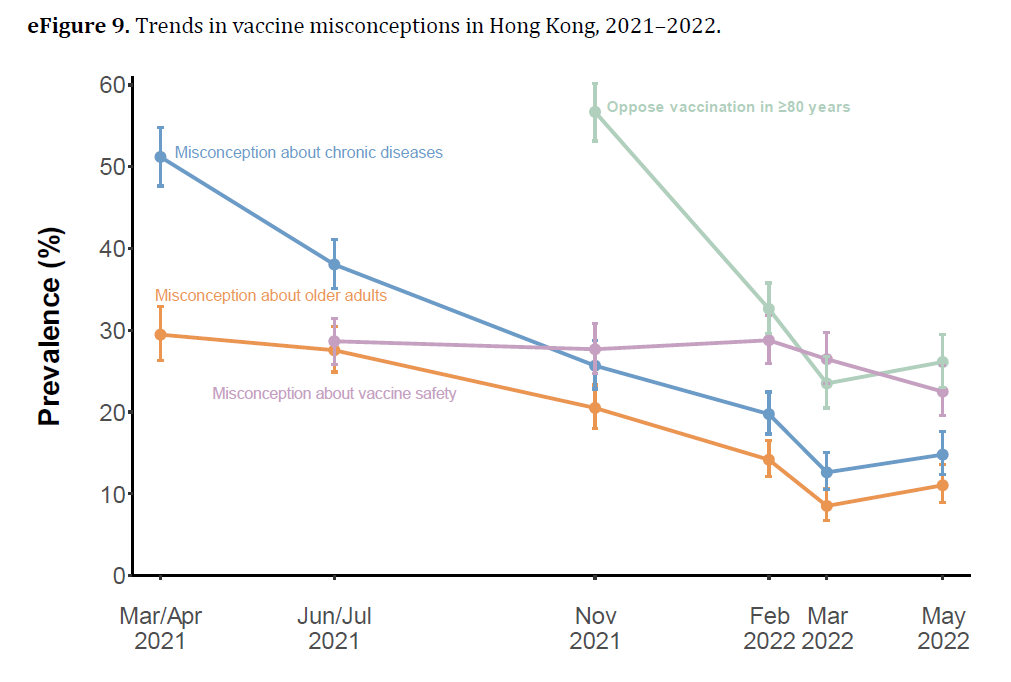
Over half of the adult population (59%) in Hong Kong reported a major misconception about COVID-19 vaccines. In contrast, this number was 17% in in Singapore (Figure A below). Somewhat incredibly, at one point 57% of participants in Hong Kong opposed vaccination in adults aged 80 years and older, the age group that accounted for most COVID-19 deaths (see eFigure 9).
Figure B below shows the relative trust in different sources of information, which may be compared with a parallel assessment Singapore, where much higher trust overall was observed.

Figure 4. COVID-19 Vaccine Misconceptions and Trust in Information Sources in Hong Kong (June to July 2021) and Singapore (May 2020 to June 2021)
While opposition to vaccination went down over time (eFigure 9), these misconceptions may have had an influence on vaccine uptake in older adults, which was abysmal (eTable 1), leading to the horrendous death rate when the Omicron wave hit.

Vaccine refusal in adults aged 18–59 years was attributed to low vaccine confidence with regards to safety, effectiveness, and their and importance, and was also influenced by political views, distrust in the WHO, government health authorities and academics. In adults aged 18–59 years, building vaccine confidence with regard to the safety, effectiveness, and
importance of COVID-19 vaccines was analyzed to potentially change vaccine refusal rates by about 9%. Addressing mistrust in the WHO, health authorities and academics could move the needle a further 5%. Shifting political views could reduce refusal by 7% (adults aged 18-59) and 5% (ages >60 yrs).
Lessons and Interpretation
Examining international studies of vaccine acceptance and uptake allow us to look at data from our own countries with a different lens. This study of Hong Kong residents examined the shift in vaccination willingness from before vaccine distribution, to widespread vaccination. It identified the significant influence of political ideologies on both short-term and long-term COVID-19 vaccine hesitancy. Importantly, the researchers found that a substantial portion (about 73%) of the relationship between political views and vaccine refusal could be influenced by factors that may be changeable, such as mistrust in health authorities, low confidence in vaccines, and misconceptions about vaccines. This gives important lessons for public health organization and health professionals everywhere. If you’re a health care professional, your relationship with your patients may make an important difference in your patient’s vaccination willingness. Health care professional attitudes may have had an effect in Hong Kong. The authors noted that many physicians were unvaccinated and were also significant sources of vaccine misinformation. Clearly, attitudes can outweigh expected science literacy. If health care professionals aren’t convinced, their patients likely won’t be, either.
About 59% of adults in Hong Kong held at least one misconception about COVID-19 vaccines, substantially more that Singapore. As has been discussed elsewhere, even brief exposure to misinformation may impact vaccine perceptions. In this case, one in four adults in Hong Kong believed that COVID-19 vaccines posed a greater risk than the infection itself, a belief that persisted for a year, despite Hong Kong experiencing the world’s highest daily COVID-19 mortality rates at one point. How we can “vaccinate” against vaccine misconceptions is an open question, perhaps for another post. The authors suggest that building trust is key. Fostering trust in health authorities, government health agencies, and academic institutions could support “resistance” against misinformation and misconceptions with also supporting vaccine update and confidence. While I am a layperson and non-expert when it comes to Hong Kong, it appears the fractious relationship between residents and the government over the past several year may have led to a significant effect on confidence and trust, which led to deep skepticism of the COVID-19 vaccination campaign. Less than half of adults (47%) expressed trust in their government health authorities regarding COVID-19 vaccines, compared with 91.0% of adults in Singapore.
Where vaccine refusal is widespread, the authors argue that the primary explanations are more likely to be related to systemic, overarching factors rather than individual characteristics. They identified four key factors that they believe accounted for 75% of vaccine refusal among adults. While political views were found to be a contributing factor, they were not the primary cause. While mandates drove uptake in younger adults, they did not drive residential care resident and elderly vaccinations (and it did not appear there was a specific campaign to vaccinate this population).
Conclusion
This study offers a comprehensive examination of COVID-19 vaccine refusal in Hong Kong. It identifies potential factors contributing to Hong Kong’s low vaccination rates and identifies the challenges that face public health organizations in Hong Kong, with lessons for health care professionals and public health worldwide.
Trust is key. Trust in health authorities, health professionals and public health agencies, with trusted messengers to build confidence are lessons that extend beyond Hong Kong. Thinking about the bruising that public health agencies took during the pandemic (and the criticism they continue to face), highlights the challenge we face as we continue to deal with this pandemic while starting to prepare for the next one.

